The current snapshot of overall health in the U.S. isn’t the greatest. From preventable chronic conditions to mental health difficulties, we’re spending more than ever, but the problems aren’t really getting any better.
Instead, there is a lot of finger-pointing that goes on between payers, providers, and patients. Truthfully, all are equally accountable.
The growing recognition that mental health and physical health are inextricably part of the same whole person is a step in the right direction. However, much of this system still then relies on fee for service model requiring a diagnosis and a billable code for reimbursement.
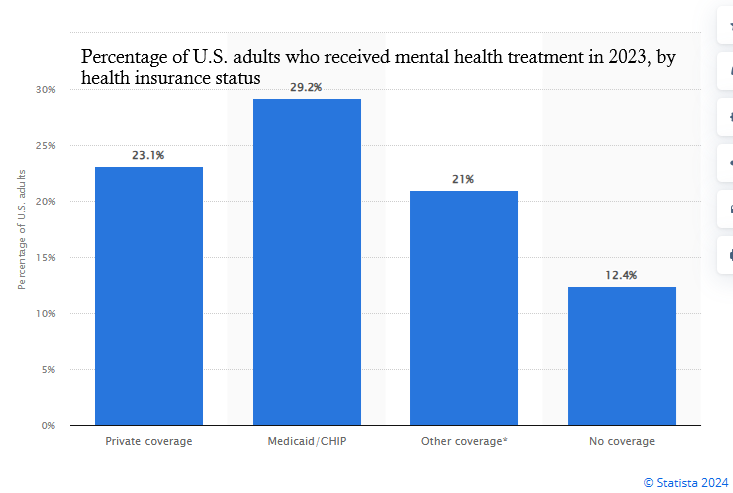
Improving mental health improves physical health and bolsters the immune system. Reducing stress, loneliness and anxiety while creating more connection, support and resilience has a significant impact on mental and physical health. These don’t require CPT codes or HCPCS or co-pays or deductibles. A new system of subclinical support is emerging that puts the power (and dollars) back into the hands of the consumers and they payers, while allowing providers to focus on the more acute clinical needs.
According to the American Academy of Family Physicians (AAFP), up to 75% of primary care visits include mental or behavioral health components. Three quarters of the people are experiencing emotional or psychological stress. Layering our services on as systemic connector to help fill the gaps between primary care and clinical mental health services just makes sense.
Moving away from a sick care system is essential for population health. Focusing on prevention, healthy maintenance/lifestyle, relationships/connection, purpose, exercise and mindset, to name a few, would have a dramatically more positive impact on the human race than over-prescribing and over-pathologizing. Unfortunately, simple tools people can apply at home don’t pay as much, so our system isn’t designed to promote them as much. Instead of arguing over who should pay for GLP-1s and SSRIs and how much they cost, how about we focus on preventing the need for them and reducing the effects of negative stress instead?
Stress, Chronic Illness & Loneliness
The relationship between stress and chronic illness has been proven by decades of research. Helping people to build resiliency can reduce cardiovascular and gastrointestinal issues, hypertension, diabetes, fatigue, and more.
In addition to physical illness are also the mental health conditions that can be created by overwhelming stress, such as anxiousness and depressive mood.
The U.S. Surgeon General also recently released an advisory report called “The Epidemic of Loneliness and Isolation” This report shows how desperately people around the country need connection with others, and how healthier and more supportive digital resources are needed to foster growth. Innovia’s platform speaks directly to solve many of the needs outlined in this advisory.
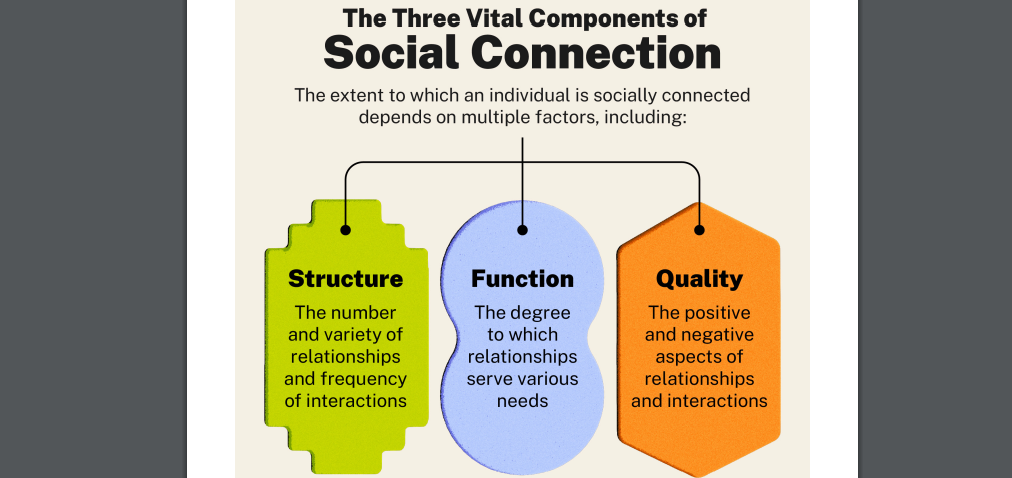
Here is a selection from the report: “Loneliness is far more than just a bad feeling—it harms both individual and societal health. It is associated with a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death. The mortality impact of being socially disconnected is similar to that caused by smoking up to 15 cigarettes a day, and even greater than that associated with obesity and physical inactivity. And the harmful consequences of a society that lacks social connection can be felt in our schools, workplaces, and civic organizations, where performance, productivity, and engagement are diminished.
Loneliness and isolation represent profound threats to our health and well-being. But we have the power to respond. By taking small steps every day to strengthen our relationships, and by supporting community efforts to rebuild social connection, we can rise to meet this moment together. We can build lives and communities that are healthier and happier. And we can ensure our country and the world are better poised than ever to take on the challenges that lay ahead.
Our future depends on what we do today.”
Layering in Subclinical Support
In the words of an astute colleague who is also a therapist and teacher, “You can get clinical results from subclinical solutions.”
Not everyone needs to see a therapist, many are overloaded already. In fact, most people don’t need clinical interventions to help relieve stress or solve difficulties they’re having in life. Peer support, coaching, mentoring, education, and experiential leadership are essential for making progress en masse. When done in groups, people feel a sense of belonging when they realize they’re not alone in their journeys and can support one another.
According to the Mayo Clinic, participating in support groups provides people with an opportunity to be with others who are likely to have a common purpose and likely to understand one another. Some of the benefits include:
• Feeling less lonely, isolated or judged
• Reducing distress, depression, anxiety or fatigue
• Talking openly and honestly about your feelings
• Improving skills to cope with challenges
• Staying motivated to manage chronic conditions or stick to treatment plans
• Gaining a sense of empowerment, control or hope
• Learning about health, economic or social resources
Everyone needs support and connection with like-minded people throughout their lives, and our services are geared to provide this to a cross section of society and walk with them to meet various needs and challenges over a long period of time. We offer services to everyday people, whether or not they ever become consumers of traditional behavioral health treatment or therapy. We also help in settings where we can provide extra support in between therapy visits, primary care visits, and more, while increasing engagement, improving health conditions, and lowering overall costs.
As an example of the effectiveness of groups led by peers, Mental Health America highlights studies that this type of support by saying, “Peer support is an evidence-based practice for individuals with mental health conditions or challenges. Both quantitative and qualitative evidence indicate that peer support lowers the overall cost of mental health services by reducing re-hospitalization rates and days spent in inpatient services, increasing the use of outpatient services. Peer support improves quality of life, increases and improves engagement with services, and increases whole health and self-management.”
Adding more engagements per month and over longer periods of time helps improve outcomes for:
– ACOs
– MCOs
– CCBHCs
– Employers
– SUD/MH/MAT providers
– Universities
– Digital Health providers
– and more…
Save Money and Improve Overall Health
By reducing stress and building connection and resilience, people become happier and healthier. This is what we’re built for – addressing a variety of needs throughout ongoing challenges in life.
Happier and healthier people show up more and perform better at work and have a more positive impact in their personal and professional relationships.
Happier and healthier people have less associated medical and behavioral health costs.
Happier and healthier people make more progress in their weekly therapy sessions by having support in between or reducing the number of therapy sessions.
Our customizable support services help unburden the system while saving money and improving overall health. It’s literally win-win-win.